What Is AMH? When you start planning for a baby, there are so many new medical terms that suddenly become part of your world — ovulation, ovarian reserve, fertility tests, and one of the most common among them is AMH. Many women hear about AMH for the first time when their gynecologist suggests an AMH test. Naturally, this leads to questions: What is AMH? Why is it important? Does a low AMH level mean I can’t get pregnant?
If you’ve been wondering about these things, you’re not alone. Let’s break it down in simple words so you feel empowered and informed about your reproductive health.
What is AMH?
AMH stands for Anti-Müllerian Hormone. It is a hormone produced by small fluid-filled sacs in your ovaries called follicles. Each follicle has the potential to grow into a mature egg, and the amount of AMH in your blood gives doctors an idea of how many eggs you might have in reserve.
In other words, AMH is like a mirror reflecting your ovarian reserve. A higher AMH suggests that you have more eggs left, while a lower AMH indicates fewer eggs. This is why doctors often recommend an AMH test for women who are planning pregnancy, facing irregular cycles, or considering treatments like IVF.
Why is AMH Important?
When we talk about fertility, two things matter:
- Egg quantity – how many eggs you have left in your ovaries.
- Egg quality – how healthy those eggs are.
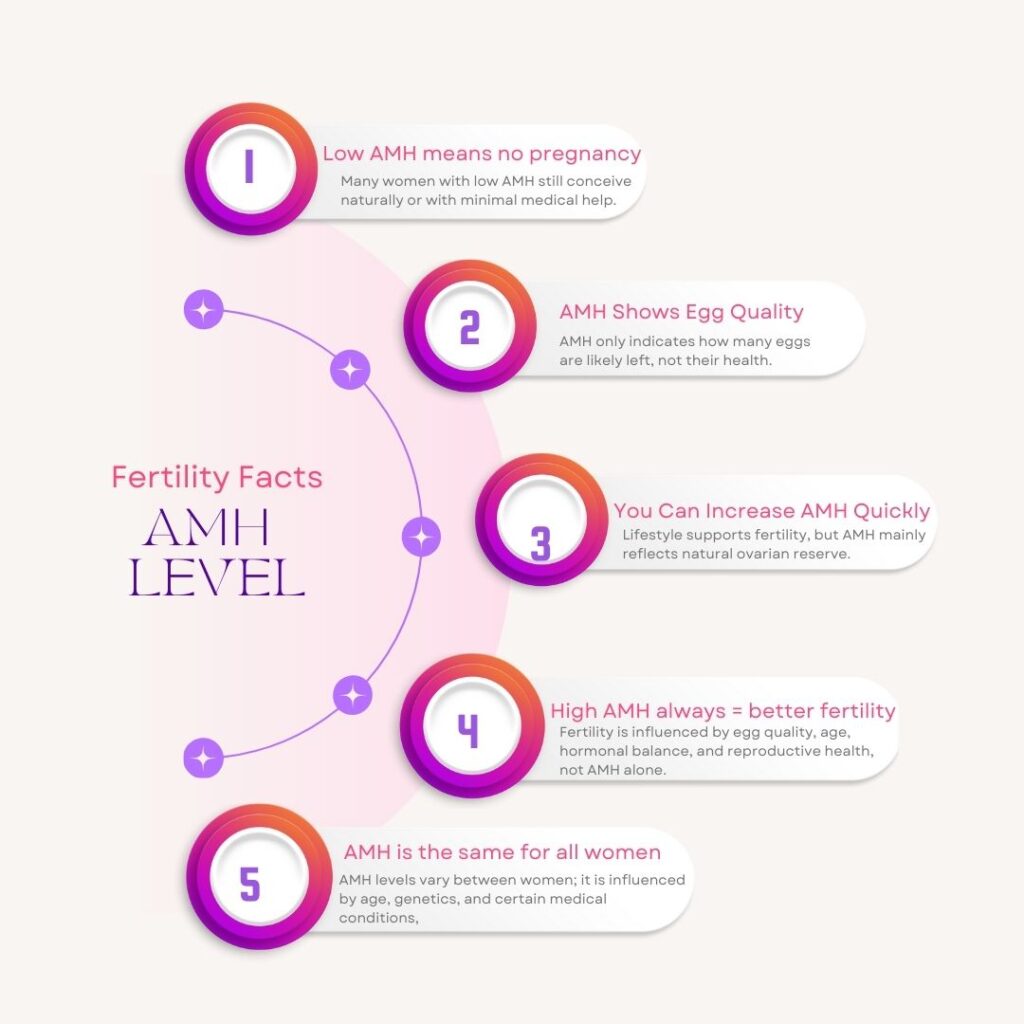
AMH gives an insight into the quantity, not the quality. This means that even if you have low AMH, it doesn’t automatically mean you cannot conceive. Many women with low AMH still become pregnant naturally, while some with normal AMH may face challenges. It’s just one piece of the larger fertility picture.
Normal AMH Levels
While levels vary depending on the lab and your age, doctors often use these general ranges (in ng/ml):
- High AMH: More than 4.0 (sometimes linked with PCOS, where ovaries produce more follicles).
- Normal AMH: 1.5 – 4.0 (a healthy ovarian reserve).
- Low AMH: 1.0 – 1.5 (fewer eggs in reserve, but conception is still possible).
- Very Low AMH: Below 1.0 (ovarian reserve is significantly reduced).
It’s important to remember that AMH naturally declines with age. A 28-year-old with an AMH of 1.0 might still have a better chance of conceiving than a 38-year-old with the same number, because egg quality decreases with age even if quantity is similar.
AMH in Relation to Age
Since women are born with all the eggs they’ll ever have, AMH levels decline naturally with age. Understanding this decline helps put your numbers into perspective.
Here’s a general age-wise reference (values may vary by lab and individual):
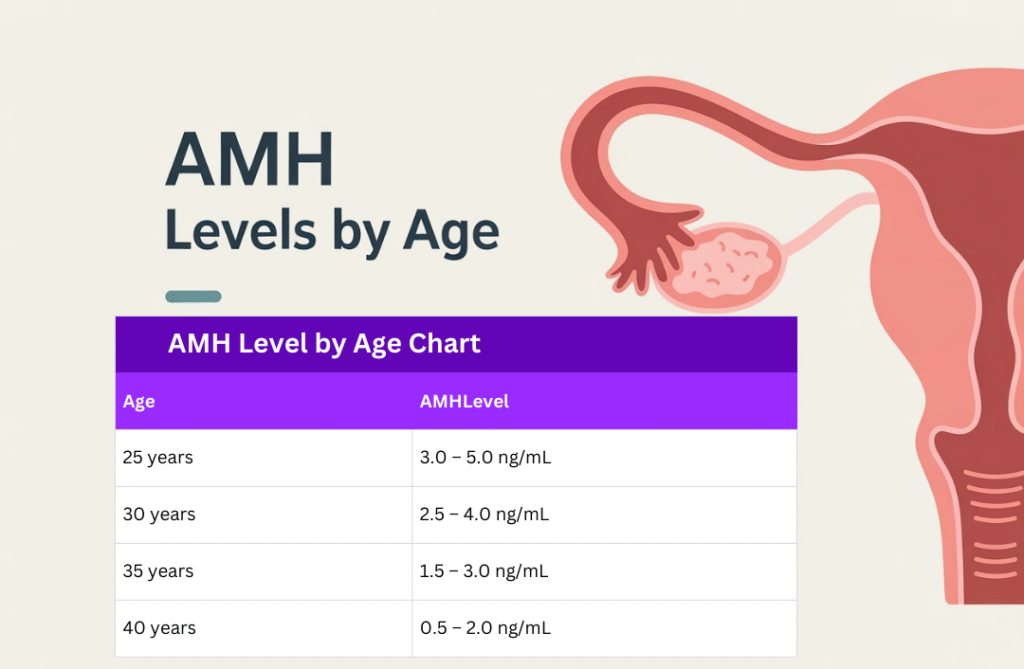
This table shows why AMH is often tested in women who want to delay pregnancy or are considering egg freezing. The earlier you know your ovarian reserve, the better you can plan.
Why Do Doctors Suggest an AMH Test?
An AMH test is a simple blood test that can be done at any time during your menstrual cycle. Doctors may recommend it for several reasons:
- If you’ve been trying to conceive for a while without success.
- If you’re planning to delay pregnancy and want to know your fertility status.
- If you’re considering egg freezing or IVF.
- To check for conditions like PCOS or premature ovarian failure.
The test helps doctors plan your fertility journey more effectively. For example, in IVF treatment, knowing AMH levels can help predict how your ovaries might respond to stimulation medicines.
What is AMH Test?
The AMH test is a simple blood test that can be done on any day of your menstrual cycle. This makes it very convenient compared to other fertility hormones like FSH or LH, which need to be measured on specific cycle days.
- Fasting is not required before an AMH test.
- The procedure is quick, usually just a regular blood draw.
- Results are typically available within 24–48 hours, depending on the lab.
This test can be done at any standard diagnostic center and is often one of the first steps recommended if you’re planning pregnancy or consulting a fertility specialist.
AMH and Fertility Treatments
Doctors often use AMH levels as a guide in fertility treatments:
- IVF (In Vitro Fertilization):
AMH helps predict how your ovaries will respond to stimulation injections. Women with higher AMH may produce more eggs, while women with lower AMH may need tailored doses to optimize egg retrieval. - Egg Freezing:
AMH is crucial in deciding the right time to freeze eggs. Women in their late 20s to early 30s with good AMH levels are often the best candidates, as it indicates both egg quantity and younger egg quality.
In short, AMH helps fertility specialists customize your treatment plan instead of following a one-size-fits-all approach.
Limitations of the AMH Test
While AMH is a valuable marker, it’s important to understand its limitations:
- Doesn’t predict natural conception: Some women with low AMH conceive naturally, while others with normal AMH may face challenges. Fertility is influenced by many factors — egg quality, fallopian tubes, sperm health, and overall reproductive wellness.
- Lab variations: AMH results can vary slightly depending on the testing method or lab standards. That’s why interpretation should always be done by a fertility specialist.
- Not a complete picture: AMH is just one piece of the fertility puzzle. Doctors usually combine it with ultrasound scans (antral follicle count) and other hormone tests for a more accurate assessment.
Myths and Facts About AMH
There’s a lot of confusion around AMH, so let’s clear it up:
What Affects AMH Levels?
Several factors influence AMH:
- Age – AMH naturally decreases as you get older, especially after 35.
- Genetics – Some women are born with fewer eggs.
- Medical conditions – Endometriosis, autoimmune diseases, and certain treatments (like chemotherapy) can lower AMH.
- Lifestyle factors – Smoking, poor diet, or extreme stress may also impact ovarian health.
Can Lifestyle Improve AMH?
Strictly speaking, AMH is not a number you can easily change. However, a healthy lifestyle can improve your overall fertility and the quality of your eggs, which is equally important. Here are some tips:
- Eat a balanced diet with leafy greens, whole grains, proteins, nuts, and seeds.
- Include antioxidant-rich foods like berries and pomegranate.
- Maintain a healthy body weight.
- Exercise moderately — yoga, walking, or light workouts.
- Get enough sleep and manage stress.
- Avoid smoking, alcohol, and excessive caffeine.
Think of it this way: You may not be able to add more eggs, but you can nurture the eggs you have to give yourself the best chance of a healthy pregnancy.
When Should You See a Doctor?
If you’re under 35 and have been trying to conceive for more than 12 months (or more than 6 months if you’re over 35), it’s a good idea to consult a fertility specialist. A doctor can guide you with the right tests, which might include AMH, ultrasound, and hormone evaluations.
If your AMH is low, don’t panic. Doctors often suggest tailored treatments depending on your situation, which could range from natural conception support to advanced fertility options.
HugMumma’s Take
At HugMumma, we know how overwhelming fertility journeys can feel. Words like “low AMH” or “ovarian reserve” can sound scary, but remember: numbers do not define your motherhood journey. AMH is just one marker of fertility, not the final answer.
Many women with low AMH go on to have healthy pregnancies. With the right guidance, lifestyle support, and medical care, your dream of becoming a mother is still very much possible.
If you’ve just discovered the term and are wondering “What is AMH?”, take a deep breath. It’s simply a tool — not a verdict. Stay informed, stay positive, and most importantly, remember that you are not alone on this journey.








One Comment